Authored by Megan Redshaw, J.D. via The Epoch Times (emphasis ours),
People with a history of uveitis may experience a recurrence of the eye inflammatory disorder following COVID-19 vaccination, especially in the early postvaccination period.
A recently published study in JAMA Ophthalmology found that about 17 percent of nearly 474,000 vaccinated individuals with a history of uveitis experienced a recurrence within one year after vaccination.
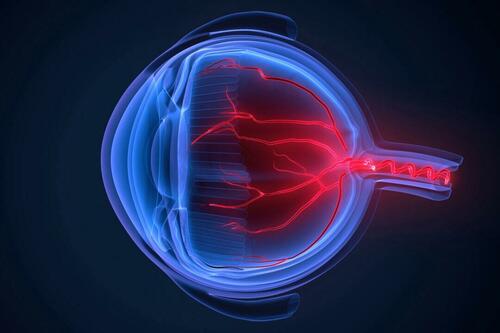
Uveitis is inflammation inside the eye that occurs when the immune system is fighting an infection or attacks healthy tissue in the eyes. It can cause symptoms including pain, redness, and vision loss while damaging the uvea and other parts of the eye.
Researchers collected data on all individuals diagnosed with uveitis in South Korea between January 2015 and February 2021 to determine the risk of recurrence after COVID-19 vaccination. Data was retrieved from the Korean National Health Insurance Service and Korea Disease Control and Prevention Agency databases. The incidence of uveitis was assessed from Feb. 26, 2021, to Dec. 31, 2022. The cases were classified according to the onset at three months, six months, and one year, the type of uveitis (anterior or nonanterior), and vaccine type.
Individuals included in the study received at least one dose of a COVID-19 vaccine from Pfizer, Moderna, AstraZeneca, or Johnson & Johnson and did not test positive for SARS-CoV-2 during the study period.
Study Findings
Of the 473,934 individuals included in the study, the cumulative incidence of postvaccination uveitis was 8.6 percent at three months, 12.5 percent at six months, and 16.8 percent at one year—primarily of the anterior type, which affects the iris at the front of the eye. Moreover, the risk of uveitis reoccurrence was highest in the first 30 days after vaccination, peaked between the first and second vaccine doses, and decreased with subsequent vaccinations.
According to the researchers, the first dose of the vaccine may activate inflammatory pathways leading to initial inflammation in people who are prone to autoimmune reactions or have a history of uveitis. However, there’s a declining risk with repeated vaccination that may be due to the immune system’s adaptation to the vaccine antigen, although further studies are needed to confirm this hypothesis.
Additionally, the risk of experiencing the condition increased among recipients of all four vaccine types, especially among those who received Pfizer’s COVID-19 vaccine. These patients were more likely to experience uveitis recurrence during the early-onset period. Likewise, those who received Moderna were at a higher risk of experiencing uveitis after the first vaccination and during the early-onset period.
Notably, there were variations in the types of uveitis observed in the periods before and after vaccination. Among patients with infectious uveitis prior to receiving a COVID-19 vaccine, nearly 54 percent had noninfectious uveitis after being vaccinated, whereas most of the individuals with noninfectious uveitis before vaccination had a recurrence of the same type after vaccination.
Most patients with uveitis were 60 to 79 years old, followed by those aged 40 to 59. Among those with comorbidities, high blood pressure, diabetes, and rheumatic diseases were the most common.
“Although uveitis following vaccination is rare, our findings support an increased risk after COVID-19 vaccination, particularly in the early postvaccination period,” the authors wrote. “These results emphasize the importance of vigilance and monitoring for uveitis in the context of vaccinations, including COVID-19 vaccinations, particularly in individuals with a history of uveitis.”
Other Studies of Vaccine-Associated Uveitis
Other studies have found an association between uveitis and COVID-19 vaccination, including a February 2023 study published in Ophthalmology. The study provided insights into a possible temporal association between reported vaccine-associated events and SARS-CoV-2 vaccines from Pfizer, Moderna, and Johnson & Johnson.
Moreover, ocular adverse events have been reported following COVID-19 vaccination in addition to uveitis, including facial nerve palsy, retinal vascular occlusion, acute macular neuroretinopathy, thrombosis, and new-onset Graves’ disease.
In a June 2022 paper published in Vaccines, researchers analyzed ocular adverse events reported to the Vaccine Adverse Event Reporting System (VAERS) to provide clinicians and researchers with a broader picture of ocular side effects of COVID-19 vaccinations.
VAERS is a voluntary reporting system comanaged by the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention. It is designed to detect vaccine safety signals, although it is estimated to represent less than 1 percent of actual adverse events.
During the analysis period of December 2020 to December 2021, VAERS received 55,313 reports for ocular adverse events, 6,688 of which met the inclusion criteria. Of those reports, 2,229 were related to eyelid swelling, ocular hyperemia, and conjunctivitis, 1,785 were reports of blurred vision, and 1,322 were reports of visual impairment.
Females accounted for 74 percent of the reports, and eye conditions affected primarily individuals between the ages of 40 and 59 who had received either the Johnson & Johnson shot or Moderna’s vaccine.
Of the patients who reported ocular-related complications, 50 percent received Pfizer’s COVID-19 vaccine, 38 percent received Moderna, and 12 percent received the Johnson & Johnson vaccine.
Although the study’s authors said they could not determine whether the vaccines were associated with an increased risk of adverse events, their data suggests a “possible association between COVID-19 vaccines and ocular adverse events.”
“Physicians are cautioned not only to be aware of this potential problem, but to check any underlying patient conditions, and to carefully document in VAERS within a few weeks of vaccination,” they wrote.
According to current VAERS data, 734 cases of uveitis, 539 cases of eye inflammation, 2,781 cases of retina disorders, 11,641 cases of facial nerve disorders, and 3,909 reports of eyelid swelling, ocular hyperaemia, and conjunctivitis were reported following COVID-19 vaccination between Dec. 14, 2020, and March 29.
Potential associations between uveitis and other vaccinations have been reported, including influenza, human papillomavirus, and varicella zoster virus vaccines. However, these studies did not necessarily establish a causal link.