People with a leading cause of blindness were able to read again thanks to a tiny wireless chip implanted in the back of the eye and specialized augmented glasses, according to study results published Monday in the New England Journal of Medicine.
The trial involved 38 European patients, all of whom had an advanced stage of dry age-related macular degeneration (AMD) known as geographic atrophy.
There is no cure for AMD, which is driven by changes in a part of the retina called the macula and caused by inflammation and a build-up of waste. The photoreceptor cells in the macula are responsible for producing sharp, detailed and colored vision. When the disease has progressed to the geographic atrophy stage, the cells deteriorate and die, and people lose their central vision — meaning an object straight ahead may appear blurry or covered up with a dark blotch.
Roughly 22 million people in the United States have AMD, and about 1 million have geographic atrophy, according to the American Macular Degeneration Foundation.
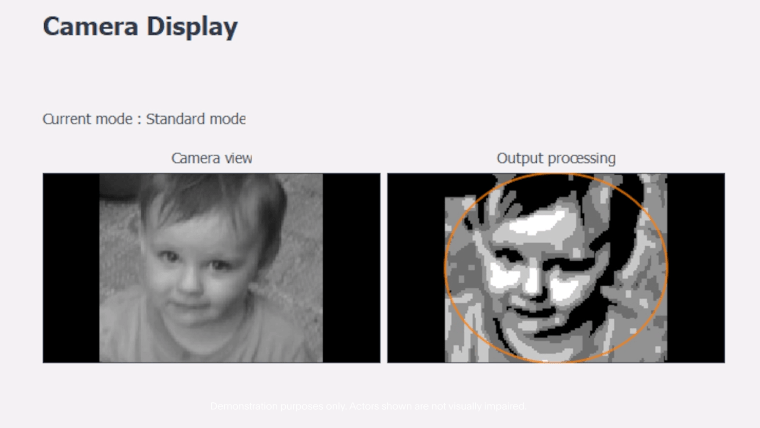
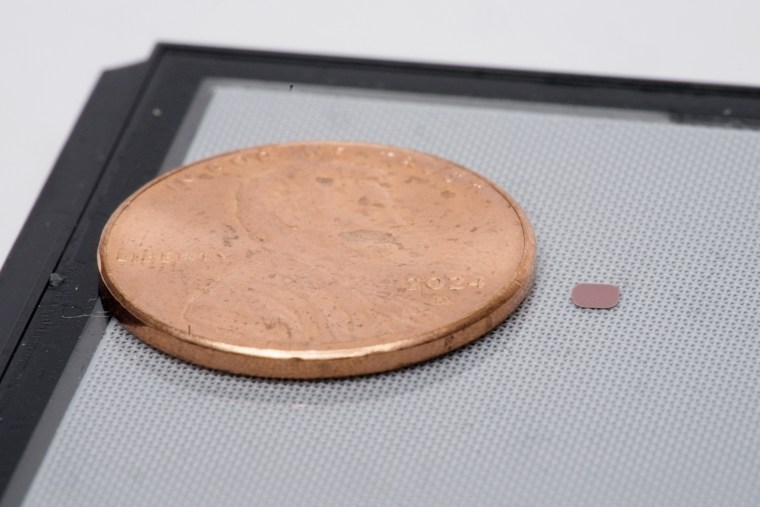
In the study, the participants, who had an average age of 79, were fitted with the “PRIMA device,” a system meant to replicate vision. Patients wear augmented reality glasses embedded with a camera that captures their visual field. What the camera “sees” is transmitted to the chip implanted in the eye in the form of infrared light. The chip converts the light into an electrical current, which stimulates the remaining healthy cells in the macula in a realistic way, enabling the brain to interpret signals the cells send as vision.
An image processor, which users must carry, lets patients zoom in and magnify the images they see, which appear in black and white.
With the help of the PRIMA device, 80% of the 32 patients who returned for reassessments one year after the chip implantation had achieved clinically meaningful visual improvements. Patients did experience side effects, predominantly related to the surgical procedure: The study reported that 26 serious adverse events occurred in 19 of the patients, ranging from elevated blood pressure in the eye to an accumulation of blood around the retina. The majority of the adverse events resolved within two months of the implantation.
“It’s the first ever therapeutic approach that has led to an improvement in visual function in this group of patients,” said Dr. Frank Holz, the trial’s lead investigator and chair of the department of ophthalmology at the University Hospital of Bonn in Germany. “Late-stage age-related macular degeneration is a dismal disease. Patients are no longer capable of reading, driving a car, watching TV or even recognizing faces. So [these results] are a game changer in my mind.”
One patient, Sheila Irvine, 70, who was fitted with the PRIMA device at Moorfields Eye Hospital in London, said in a statement provided by the hospital that her life before she received the implant was akin to “having two black discs in my eyes, with the outside distorted.” A self-described “avid bookworm” before she lost her vision, Irvine said she was now able to do crosswords and read prescriptions.
Dr. Sunir Garg, professor of ophthalmology at the retina service of Wills Eye Hospital in Philadelphia, who was not involved in the study, said the results are a breakthrough for patients with geographic atrophy. All doctors have been able to offer, he said, are visual aids, like magnifiers, and emotional support.
“Even with new medical therapies, the best that we can do is slow it down,” said Garg, who works with several drugmakers involved in treatments for AMD, including Apellis Pharmaceuticals, the maker of pegcetacoplan. The drug, which slows the progression of geographic atrophy, was recently approved in the United States and must be injected into the eye every one to two months. “We can’t stop it, and we can’t do anything to bring back lost vision.”

Dr. Demetrios Vavvas, director of the retina service at Mass Eye and Ear in Boston, who was also not involved in the study, said the PRIMA system is not without limitations.
Vavvas noted that the surgery required to implant the chip in the eye requires a high level of surgical skill and is not without risk. “You have to lift the retina off its normal position to implant this device, which increases the atrophy,” said Vavvas, who is a consultant to Sumitomo Pharmaceuticals, a company working on stem cell therapies for patients with other forms of vision loss.
Vavvas said it was important to note that the device is not restoring normal vision, as patients were able to see only in black and white rather than color, and that the trial participants had to undergo a significant amount of training to learn how to see with the device. He also said it was not clear whether the enhancements in visual ability had significantly improved the patients’ quality of life.
But at the same time, Vavvas was also optimistic about its potential, describing the current iteration of PRIMA as a key steppingstone in the field of vision restoration.
“Think of this device as the pre-release iPhone,” he said. “The limitations are clear. We shouldn’t oversell that the quality of life really improved. But there were certain [visual] tasks at which the patients were clearly better. So it shows to us that there is potential in this approach. It is still, in some ways, a prototype. They’re working on iterations of this device that will be better.”
New upgrades to the device could be coming in the next couple of years.
The PRIMA system was invented by Stanford University ophthalmology professor Daniel Palanker and is being developed by the California-based neural engineering company Science Corp.
Palanker said technical improvements are being made to increase the number of pixels in the chip from 400 to 10,000. The new chips have already been tested in rats, and the upgraded chips are being manufactured for future human trials. With the aid of the camera’s zoom function, Palanker said, that could theoretically enable patients to achieve 20/20 visual resolution.
“We are also working on next-generation software that will allow patients to perceive not just black-and-white text, but also gray-scale natural images, such as faces,” Palanker said.
Palanker suggested that the technology could be trialed in other retinal diseases that cause blindness, such as Stargardt disease, which has similar symptoms to age-related macular degeneration but is genetic and usually affects younger people.
Garg and Vavvas are eager to see larger trials that provide more details about how the device improves patients’ ability to function day to day. Vavvas suggested that future trials should include a control arm to understand the extent to which the device yields real-world benefits, for example compared with existing electronic magnifiers.
“Is it something that is good enough for patients to say, ‘Well, I’ve regained my independence because I can now do my credit card bills myself, stamp and address my envelopes myself, and look at grocery store labels’?” Garg said. “Those kinds of practical things I would like to know more about.”
Vavvas said: “This is a chronic disease that you will have for life, so we need more than one year of follow-up to see other risks, other problems. Does that signal of efficacy that we see at 12 months remain two years later?”
While Vavvas said he would not call the device a panacea for blindness, the study showed that brain-computer interfaces can represent an important approach to tackling different kinds of severe visual impairment. “As the iterations of this device become better and better, it could become a real solution for a cohort of patients,” he said.